How Robotic Process Automation Transforms Revenue Cycle Management (RCM)?
These days, healthcare is becoming more popular by using robots to automate human tasks in the revenue cycle. Healthcare organizations are increasingly adopting robotic process automation to automate revenue cycle tasks.
Revenue Cycle Management encompasses the entire patient journey, from appointment scheduling to billing and payment. It involves various stages, including patient registration, insurance verification, claim submission, and payment processing. Each stage is crucial for the smooth flow of revenue within healthcare organizations.
How Can RPA Improve Revenue Management in Healthcare?
RPA in healthcare is the technology that enables the automation of repetitive, rule-based tasks previously performed by humans. RPA software, or "bots," minimizes human interactions with digital systems to execute tasks such as insurance verification automation.
For example - Running a small healthcare clinic means drowning in paperwork—patient forms, insurance claims, bills, you name it. It takes a lot of time. Now, let's talk money—Revenue Cycle Management (RCM). It's about handling all the cash stuff in your clinic—from booking appointments to getting paid for your services.
In the old days, it was all manual labor. People punched in patient details, filled out insurance forms, and more. But now, meet RPA—Robotic Process Automation. Think of them as super-efficient robots. They tackle all the boring, repetitive tasks at lightning speed and with zero mistakes. With Healthcare Automation Solutions, these RPA bots streamline processes, making it easier for healthcare providers to manage their revenue cycle effectively.
Here's a sneak peek: A patient schedules a visit. With RPA on the job, a robot instantly plugs their information into the system. When it's time to bill their insurance, another bot handles the paperwork electronically. And when payment rolls in, another bot updates your records—no human effort is needed.
RCM automation with RPA is like having a dream team of helpers manage your clinic's finances, leaving you free to focus on what matters most—your patients!

RPA can automate tasks such as:
- Patient Eligibility Verification: Bots can access insurance databases to verify patients' insurance coverage and eligibility for services, reducing errors and delays in claims processing.
- Claims Processing: RPA bots can automatically generate and submit insurance claims based on patient records and treatment information, reducing the time and effort required for manual data entry.
- Payment Posting: Bots can reconcile payments received from insurance companies or patients with the corresponding claims, which updates the billing system and decreases any discrepancies for review by staff.
- Third Party Automation: Many third parties do not provide any API connections, but an RPA bot can interact with third-party systems as a human, ensuring seamless data transfer and communication within RPA for healthcare automation.
How RPA (Robotic Process Automation) for Revenue Cycle Management (RCM) can benefit your business:
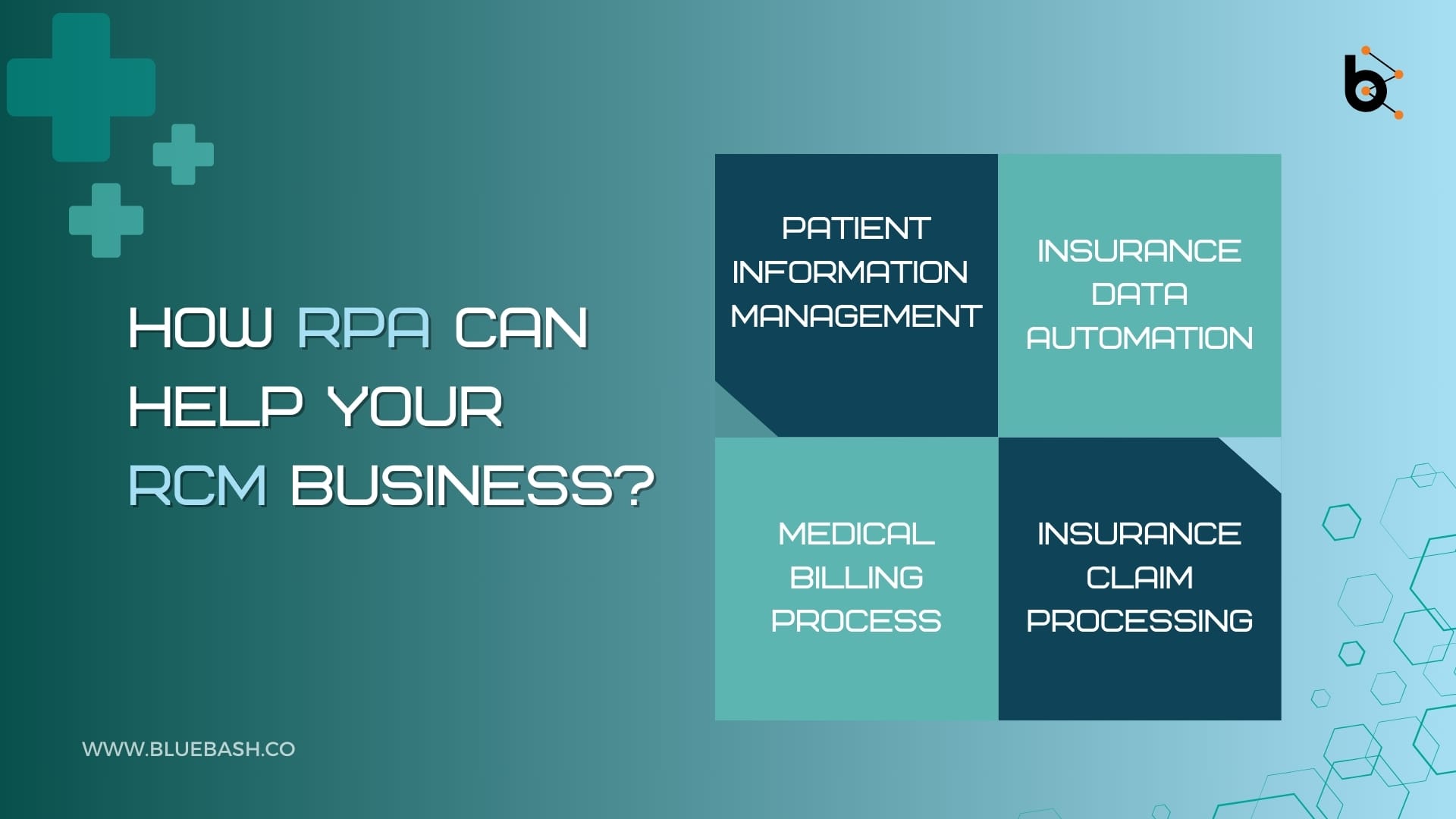
- Patient Information Management:
RPA helps manage patient information more efficiently.RPA bots can automate tasks like updating patient records, verifying their details, and keeping everything organized, which saves time and reduces errors. - Insurance Data Automation:
With RPA, the process of dealing with insurance data becomes much smoother. This includes tasks like checking insurance eligibility, verifying coverage details, and updating insurance information. RPA bots can handle these tasks quickly. - Medical Billing Process:
RPA for Medical Billing simplifies the medical billing process by automating the various tasks. This includes generating invoices, submitting claims to insurance companies, and tracking payments. RPA bots can handle these tasks efficiently, reducing the time and effort required for billing tasks. - Insurance Claim Processing:
RPA manages the process of processing insurance claims. This involves tasks like verifying claim details, checking for errors or discrepancies, and submitting claims to insurance companies. RPA bots can handle these tasks automatically to ensure that claims are processed accurately.
Benefits of Utilizing RPA for RCM
Do you know that, as per the Council for Affordable Quality Healthcare (CAQH), the adoption of revenue cycle automation for administrative tasks could yield annual savings of $17.6 billion? This figure adds to the $166 billion that the healthcare industry has already saved annually through the automation of administrative transactions. Employing RPA offers distinct advantages to healthcare providers, including:
- Enhanced Accuracy and Compliance
RPA eliminates the risks associated with human error, ensuring accurate data entry and compliance with regulatory standards such as HIPAA (Health Insurance Portability and Accountability Act). By reducing manual intervention, RCM processes become more reliable and less prone to mistakes.
- Improved Efficiency and Productivity
Automation streamlines RCM workflows, significantly reducing processing times for tasks like claims processing and payment posting. With RPA handling repetitive tasks, healthcare staff can focus on more value-added activities, leading to increased productivity and better patient care.
- Faster Revenue Cycle
By accelerating processes such as claims submission and reimbursement, RCM automation with RPA shortens the revenue cycle. Healthcare providers experience quicker payments, improving cash flow and overall financial performance.
- Cost Savings
Automating RCM tasks with RPA reduces operational costs associated with manual labor, paper-based processes, and error rectification. The efficiency gains translate into significant cost savings for healthcare organizations in the long run.
- Scalability and Adaptability
RPA solutions offer scalability to accommodate growing volumes of RCM transactions without the need for additional human resources. Moreover, they can adapt to changing regulations and requirements, ensuring continued compliance and efficiency.
6. Robotic Virtual Assistants
In healthcare organizations, having someone manage your inputs and outputs can be very helpful. Bots work as digital helpers that can be a lifesaver. For example, when an important email comes in, a bot can read it, pick out the important stuff, and send it to the right people.
- Pre-registration Capability
Bots can speed up the pre-registration process after patients fill out forms. Patients can send their information online at any time. Bots then check databases, fill in missing information on forms, and manage any issues—so everything's sorted by morning.
- 24/7 Workforce
RPA bots can work non-stop, like a digital team. As an example, the bots could receive incoming claims data from providers, evaluate it, extract required data, identify exceptions, and process invoices.

Conclusion:
In the ever-evolving landscape of healthcare finance automation, RPA emerges as a game-changer that helps healthcare providers to navigate complexities and achieve financial success while prioritizing patient well-being.
The integration of Robotic Process Automation (RPA) into Revenue Cycle Management (RCM) is revolutionizing the way healthcare organizations manage their finances and administrative tasks. By automating repetitive and rule-based processes, RPA manages operations, enhances accuracy, and improves efficiency throughout the revenue cycle.
Healthcare providers are adopting RPA solutions to optimize tasks such as patient data management, insurance data processing, and insurance claim handling. These advancements not only save time and reduce errors but also ensure compliance with regulatory standards, such as HIPAA.
FAQ's
- How does RPA benefit Revenue Cycle management (RCM) in healthcare?
RPA optimizes RCM by automating tasks such as patient data entry, insurance verification, claims processing, and payment posting. This reduces manual effort, minimizes errors, accelerates revenue cycles, and ensures compliance with regulatory standards. - What is the impact of RPA on the patient experience?
RPA integration in RCM improves the patient experience by enabling faster claim processing, more accurate billing, and smooth communication regarding insurance matters. Patients benefit from shorter wait times, reduced paperwork, and better transparency throughout the process. - How does RPA help with insurance verification in healthcare RCM?
RPA automates the process of verifying patients' insurance coverage and eligibility for services. Bots access insurance databases, retrieve relevant information, and update patient records, which minimizes claim denials. - Is RPA suitable for all healthcare organizations?
While RPA offers numerous benefits, it may not be suitable for all healthcare organizations. Factors such as organizational size, complexity of processes, existing technology infrastructure, and budget constraints should be considered before implementing RPA.